 |
 |
- Search
| Qual Improv Health Care > Volume 28(1); 2022 > Article |
|
Abstract
Purpose
We investigated physicians' responses to a series of clinical vignettes consisting of patient safety incidents, with and without disclosure of patient safety incidents (DPSI).
Methods
An anonymous survey was conducted to investigate physicians’ responses to the DPSI via online communities of physicians, and additional participants were recruited using a snowballing sampling method. We evaluated physicians’ responses to the DPSI using eight hypothetical scenarios (HS) from the following perspectives: thoughts regarding medical errors, revisiting the physician, recommendation, lawsuit, criminal prosecution, trust score, and compensation amounts. We used the chi-square test to evaluate the overall differences in response rates among the scenarios. Statistical analyses were performed using the Student's t-test to compare the trust scores and compensation amounts.
Results
A total of 910 physicians participated in this survey. An overall comparison of trust scores among HS showed that HS 1 (unclear medical errors, minor harm, and DPSI) had the highest trust score. In contrast, in the opposite scenario, HS 8 (clear medical errors, major harm, and DPSI not conducted) received the lowest scores. Cases with minor harm to patients (HS 1, 2, 5, and 6) showed lower compensation amounts than the others (HS 3, 4, 7, and 8). Physicians were more likely to think of situations with DPSI as not having medical errors (53.1% vs. 55.2%). In addition, the scenarios with DPSI were evaluated favorably in terms of intention to revisit, recommend, suit, and engage in criminal proceedings. Physicians showed higher trust scores (6.2 vs 5.4) and gave lower compensation amounts ($27.7 million vs $28.1 million), although there was no significant difference in terms of compensation amounts to the physician conducting DPSI.
Since the release of the Institute of Medicine’s crucial report (To Err Is Human) in 1999, which indicated that preventable adverse events occur in the healthcare field, patient safety has been recognized as a global public health challenge and has attracted considerable attention [1]. While multifaceted solutions have been developed to deal with patient safety incidents, including through law and culture, other strategies target incident prevention and post-management of patient safety incidents. Such incidents can lead to medical disputes depending on the communication between physicians and patients [2]. Therefore, a communication strategy to prevent miscommunication is crucial when considering the inherent risks of the healthcare process and the possibility of medical disputes regarding patient safety incidents [3].
Disclosure of patient safety incidents (DPSI) was introduced as a strategy for patient safety incidents to prevent medical disputes; it bridges the gaps between healthcare providers and patients and their family members [4,5]. DPSI is a collective process of open and honest discussions among physicians, patients, and caregivers. Its key steps include a preemptive explanation of the incident, expression of sympathy and regret for the incident, appropriate apology and compensation when necessary, and commitment to the prevention of recurrence [5-8].
Based on the experiences of Western countries, such as the USA, UK, Canada, Australia, New Zealand, and Germany, DPSI has been introduced with supportive approaches such as “apology laws” [9,10]. The effects of open and honest disclosure, as described in previous research, include strengthening the relationship between physicians and patients, the likelihood of forgiveness, and reconciliation after an adverse event, just compensation, and decreasing the likelihood of litigation [8, 11]. However, there is limited evidence of DPSI in Asian countries that considers the cultural differences in the adaptation to disclosure [7].
In the Korean cultural context, there have been investigations into the perception of DPSI in the general population and healthcare providers [4- 12]. Positive attitudes toward the DPSI were identified among the general population in a previous study that evaluated the effects of such disclosures using hypothetical situations [5]. The Korean healthcare accreditation program recently introduced the DPSI, particularly for sentinel events [13]. Furthermore, the adoption of a partial apology is under consideration in the Patient Safety Plan [14]. However, previous perception studies have revealed the fears and concerns of physicians and nurses regarding the effects of DPSI [4,12]. Therefore, we evaluated the impact of DPSI on physicians, utilizing hypothetical vignette situations consisting of components including errors, harm, and the DPSI.
We used a set of hypothetical scenarios (HSs) for clinical situations related to the DPSI developed for use within the general population for comparability. The details of the complete set of scenarios are provided in the supporting material of a previous study [5]. The eight HSs comprised three key components: clarity of medical errors, harm to the patient, and implementation of the DPSI. Patients in scenarios HS 5, HS 6, HS 7, and HS 8 had obvious medical errors (Table 1). Meanwhile, the other vignettes (HS 1, HS 2, HS 3, and HS 4) did not provide evidence of medical errors. In terms of harm to the patients, while patients experienced major harm such as irreversible brain injury in four scenarios (HS 3, HS 4, HS 7, and HS 8), the other scenarios (HS 1, HS 2, HS 5, and HS 6) consisted of minor harm to the patients. Only patients in four scenarios (HS 1, HS 3, HS 5, and HS 7) experienced DPSI regarding patient safety incidents compared to the other scenarios (HS 2, HS 4, HS 6, HS 8).
The survey participants were required to answer the following questions in each scenario: (1) Were there medical errors in this situation? (2) If I were a patient in this situation, would I revisit the physician? (3) If I were a patient in this situation, would I recommend the physician to others? (4) If I were a patient in this situation, would I want to sue the physician? (5) Should the physician be subjected to criminal prosecution? (6) How much do you trust the physician in the situation (range: 0–10)? (7) How much money should be given to the patient to compensate for his/her experience in this situation? The survey also collected information regarding participants’ sociodemographic characteristics (e.g., sex, age group).
A four-point Likert scale was provided to participants for the questionnaires, ranging from (1) strongly disagree to (4) strongly agree. A numerical rating scale of 0 to 10 was used to measure trust in physicians. Participants responded to the expected compensation amounts in Korean won, which were then converted to U.S. dollars (1,200 won per 1 USD) during the analysis.
We conducted anonymous online surveys. We recruited participants via online communities of physicians (e.g., KakaoTalk group chat) [15]. Additional participants were recruited through the snowball sampling method, wherein participants who completed the survey recommended other physicians to participate. Informed consent was obtained from all the participants before they participated in the survey. The respondents received a gift voucher with a value of 9,000 Korean won (approximately 7.5 USD). Only one response per IP address was permitted to prevent duplication.
A descriptive analysis of the participants’ sociodemographic features, including sex, age, and work experience, was conducted. We categorized scenarios depending on the clarity of medical errors, harm to the patient, and the implementation of the DPSI, and then compared the responses. The trust score and amount of compensation were calculated as the mean±standard deviation (SD). Physicians' responses based on the Likert scale were coded into binary variables (disagreeing with the question, i.e., strongly disagree and disagree, and agreeing with the question, i.e., agree and strongly agree). While the chi-square test was conducted to compare situation-specific binary responses, the scores for trust and compensation amounts were compared using the Student’s t-test. We considered a p-value of < 0.05 as statistically significant. Statistical analysis was conducted using SAS 9.4 (Version 9.4, The SAS institute Inc. Cary, N.C.). This study was approved by the Institutional Review Board (IRB) of Ulsan University Hospital (IRB number, 2018-07-003).
The proportion of males (75.6%) was higher than that of females (24.4%) among all the respondents (N=910) (Table 2). The average age of the participants was 32.3±4.5 years, where 82.2% were between 30 and 39 years old. The average duration of work experience was 6.4 years, with most participants reporting five to ten years of work experience (67.4%).
The trust scores and compensation amounts according to the individual scenarios are presented in Table 3. When the patients experienced unclear medical errors causing minor harm, and the DPSI was conducted (HS 1), respondents gave the highest trust score (7.8±1.8). On the other hand, the trust score was the lowest in HS 8 (3.2±2.3), where the patients experienced clear medical errors causing major harm without the DPSI (HS 8). The compensation amounts show slightly different trends. Regardless of the clarity of medical errors or execution of DPSI, the compensation amounts were lower in cases with minor harm to patients (HS 1, HS 2, HS 5, HS 6: $0.1 million–$0.3 million) in comparison to the other scenarios involving major harm (HS 3, HS 4, HS 7, HS 8: $14.0 million–$96.5 million). The compensation amounts also differed depending on the clarity of medical errors. For example, respondents gave higher compensation to patients experiencing clear medical errors resulting in major harm (HS 7, HS 8: $89.5 million–$96.5 million) than patients with ambiguous medical errors resulting in major harm (HS 3, HS 4: $14.0 million–$22.5 million).
Physicians judged the scenarios with distinct medical errors (HS 5, HS 6, HS 7, HS 8) as cases of clear medical errors (83.6% vs. 24.6%, p<.05) compared to those with ambiguous errors (HS 1, HS 2, HS 3, HS 4) (Figure 1A). In cases of clear medical errors, respondents thought that the patients would be more likely to sue the physician (46.0% vs. 23.5%, p<.05) and that the physician would be more likely to be subjected to criminal proceedings (19.6% vs. 4.8%, p<.05). Conversely, the proportion reporting an intention to revisit (26.3% vs. 43.1%, p<.05) or to recommend the physician to others (22.4% vs. 35.4%, p<.001) was lower in scenarios that involved clear medical errors. In terms of trust scores, physicians in situations with unclear medical errors received a higher score than physicians experiencing clear medical errors (6.7 vs. 4.9, p<.05; Figure 1B). Regarding compensation amounts, patients experiencing unclear medical errors received lower amounts than those experiencing clear medical errors ($9.2 million vs. $46.6 million, p<.05) (Figure 1C).
The response patterns related to medical harm resemble those involving medical errors. More respondents thought that scenarios with major harm (HS 3, HS 4, HS 7, HS 8) likely possessed more error-related factors than scenarios with minor harm (HS 1, HS 2, HS 5, HS 6) (57.5% vs. 50.8%, p<.05) (Figure 2A). Additionally, participants thought that physicians in situations related to major harm were more likely to be sued (56.0% vs. 13.5%, p<.05) and subjected to criminal prosecution (18.7% vs. 5.7%, p<.05) than those in situations related to minor harm. On the other hand, a lower likelihood of revisiting (15.1% vs. 54.4%, p<.05) and recommending a doctor (12.6% vs. 45.2%, p<.05) was reported in cases of major harm. Physicians related to minor harm were given higher trust scores than those associated with major harm (6.8 vs. 4.8, p<.05) (Figure 2B). In terms of compensation, physicians thought that much more compensation should be given to the patients who suffered significant harm, compared to those who suffered minor harm ($55.6 million vs. $0.2 million, p<.05) (Figure 2C).
The response patterns to the DPSI were slightly different from those related to medical errors or harm. When physicians provided disclosure (HS 1, HS 3, HS 5, and HS 7), respondents thought the case was less likely to be an error (53.1% vs. 55.2%) (Figure 3A). Additionally, physicians providing DPSI were considered less vulnerable to lawsuits (33.2% vs. 36.2%, p<.05) or criminal proceedings (10.5% vs. 13.9%, p<.05). Conversely, intentions to revisit or recommend were higher in the scenarios that provided DPSI (intention to revisit 38.9% vs. 30.6%, p<.05; intention to recommend 32.2% vs. 25.6%, p<.05). Concerning the trust score, physicians who provided disclosure received a significantly higher score than those who did not (6.2 vs. 5.4, p<.05) (Figure 3B). The average compensation amount was also lower in situations with DPSI execution than in situations with no DPSI execution, although the difference was insignificant ($27.7 million vs. $28.1 million) (Figure 3C).
In this study, we evaluated the impact of DPSI on physicians using vignettes to support evidence of the effectiveness of DPSI. Our results showed how Korean physicians perceived the effects of the DPSI in the case of patient safety incidents. Similar to the public perception of DPSI, while physicians were more willing to revisit or recommend the practitioner when DPSI was provided in situations of patient safety incidents (HS 1, HS 3, HS 5, HS 7 vs. HS 2, HS 4, HS 6, HS 8), they were considered less vulnerable to lawsuits and criminal proceedings [5]. In addition, the average trust score was higher in the scenarios with DPSI execution than in the other scenarios. However, there was no statistical difference in the perception of medical errors and compensation amounts, depending on the provision of DPSI.
A recent systematic review of the effect of DPSI reported optimistic impacts on both the general public and healthcare providers [8]. The general public showed positive attitudes toward DPSI as follows: (1) diminished intention to file a lawsuit against healthcare providers or to punish them, (2) increased credibility of medical professionals, (3) a rise in intention to visit again or recommend physicians or hospitals, and (4) higher healthcare quality. Medical professionals also felt less guilt when DPSI was provided. However, physicians still felt pressured and expressed concerns about DPSI [16]. Owing to the prevalent doubt about the effects of DPSI among healthcare providers, DPSI has not been widely introduced in South Korea [12]. We expect that our positive results on DPSI can contribute to diminishing doubts about the effect of DPSI, particularly in South Korea.
The use of HSs might help infer the expected effects of DPSI, which is not widely distributed in the healthcare sector. A set of hypothetical scenarios, also called vignettes, is widely used in other academic fields because of the reduced response burden associated with ethical dilemmas [16]. A survey using HSs can obtain more realistic responses by imagining plausible situations than simple perception surveys can. Moreover, we can use the series of scenarios used in this study to discuss DPSI or educate various stakeholders associated with patient safety incidents. We can evaluate the effect of education by comparing responses before and after the provision of education on the DPSI.
Although our research suggested that Korean physicians were aware of the overall positive effects of DPSI in line with the previous study on the general population, no significant impact on compensation amounts was observed [5]. In a prior study of the Korean public, the execution of the DPSI reduced the amount of expected compensation by $13,641 (16,370,000 won) [5]. In this study, the average compensation amount was lower in situations with DPSI (HS 1, HS 3, HS 5, and HS 7) than in the other situations without DPSI (HS 2, HS 4, HS 6, and HS 8), though the difference was not significant ($27.7 million vs. $28.1 million). Instead, the levels of harm and clarity of the medical error appear to be more influential in determining compensation. Despite empirical evidence showing that DPSI has reduced the number of lawsuits and related costs, Korean physicians remain skeptical about whether DPSI can reduce compensation amounts [12,18,19]. Therefore, subsequent research should be conducted to analyze the number of lawsuit cases or compensation amounts through comparisons of before and after the introduction of DPSI in reality.
Physicians were more likely to assume that the scenarios had medical errors when the DPSI was not executed, although the difference was not statistically significant (HS 1, HS 3, HS 5, HS 7 vs. HS 2, HS 4, HS 6, HS 8). A prior study conducted by the Korean public found that when DPSI was not performed, people were more likely to consider the case as a medical error [5]. For laypersons, judging the presence of medical errors might be difficult due to a lack of medical background. However, physicians are more likely to decide whether a case has a medical error based on their medical knowledge in the set of scenarios. The difference in the perception of medical error between laypersons and professionals implies that honest communication is critical to prevent further disputes once a patient safety incident occurs [5,20]. Therefore, perceptions not only of the general population but also of physicians should be considered before the introduction of the DPSI.
DPSI has only been implemented by stipulating its introduction in the Patient Safety Plan and enacting an apology law to support DPSI [13,14]. Healthcare providers in clinical settings, who are closely connected to patient safety incidents, should be well prepared in considering possible changes attributed to DPSI. To promote patient safety, fostering patient safety culture is vital within the clinical field. Similarly, driving the positive attitudes of healthcare professionals should precede. We can evaluate changes in the attitudes of healthcare professionals by conducting regular surveys. Additional efforts are required, including educational programs for physicians to apply DPSI in clinical settings and to distribute DPSI [21,22].
This study has some limitations. First, physicians who participated in the online survey did not represent all physicians. A relatively large number of physicians (N=910) participated in the survey, but the participants tended to be younger because of the nature of the online survey. Thus, keeping this in mind, a similar survey of older physicians should be conducted to compare results. Second, although this study assessed the perceptions of DPSI for two types of patient safety incidents (related to surgeries and drugs) [5], it is necessary to explore the perceptions of DPSI using diverse patient safety incidents. It would also be meaningful to develop scenarios for care-related events, such as bedsores and falls, or diagnosis-related events, such as diagnostic delays and errors. Therefore, we expect further studies involving various hypothetical scenarios similar to reality in the near future.
In conclusion, we evaluated how Korean physicians perceive the impact of the DPSI on patients using a set of hypothetical scenarios. Similar to the results of prior studies, our research suggests positive perceptions of Korean physicians on DPSI. The study findings may help to spread positive perceptions and expectations regarding the effects of DPSI in Korea.
Figure 1.
Comparing scenarios according to clarity of medical errors. (A) Individual items. (B) Trust scores. (C) Expected
compensation amount. Trust score range 0–10. Compensation amounts in million U.S. dollars. *p<.05.
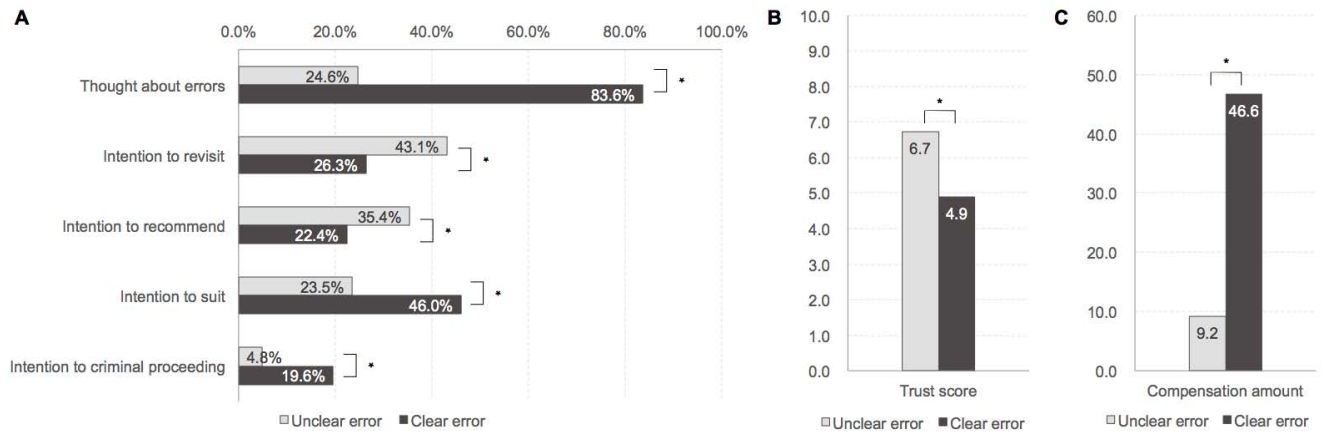
Figure 2.
Comparing scenarios with and without harm. (A) Individual items. (B) Trust scores. (C) Expected compensation amount. Trust score range 0–10. Compensation amounts in million U.S. dollars. *p<.05.

Figure 3.
Comparing scenarios with and without DPSI. (A) Individual items. (B) Trust scores. (C) Expected compensation amount. Trust score range 0–10. Compensation amounts in million U.S. dollars. *p<.05.
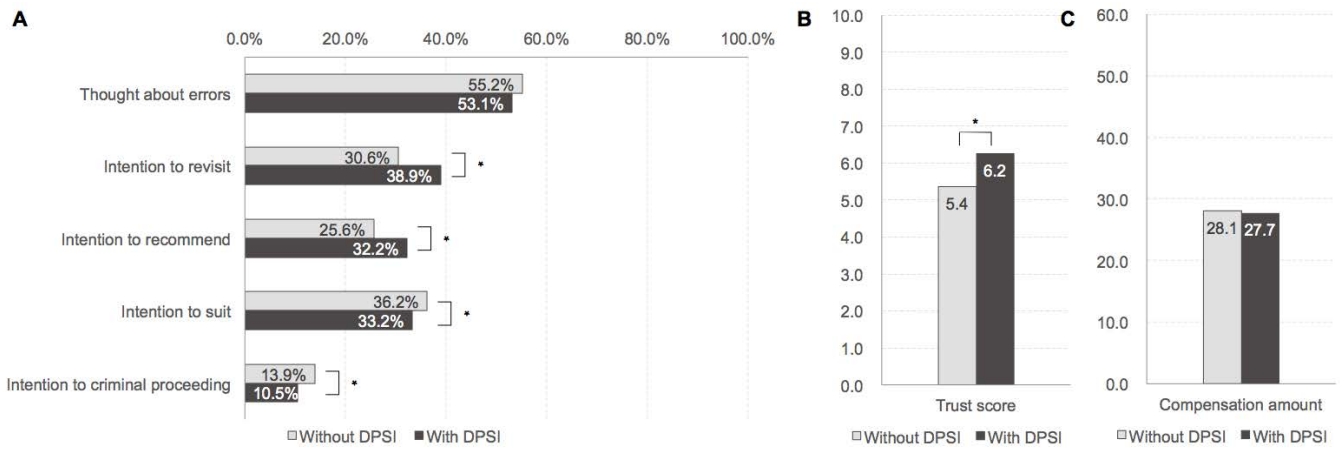
Table 1.
Characteristics of the hypothetical scenarios.
| Medical errors | Level of harm |
DPSI |
|
|---|---|---|---|
| Done | Not done | ||
| Unclear | Minor | HS 1 | HS 2 |
| Major | HS 3 | HS 4 | |
| Clear | Minor | HS 5 | HS 6 |
| Major | HS 7 | HS 8 | |
Table 2.
General characteristics of the participants.
Table 3.
Trust score and compensation amount according to hypothetical scenario.
REFERENCES
1. Leape LL, Berwick DM. Five years after To Err Is Human: what have we learned? Journal of The American Medical Association. 2005;293(19):2384-90. PMID: 15900009

2. Aoki N, Uda K, Ohta S, Kiuchi T, Fukui T. Impact of miscommunication in medical dispute cases in Japan. International Journal for Quality in Health Care. 2008;20(5):358-62. PMID: 18635588


3. Kalra J, Massey KL, Mulla A. Disclosure of medical error: policies and practice. Journal of the Royal Society of Medicine. 2005;98(7):307-9. PMID: 15994590




4. Choi EY, Pyo JH, Ock MS, Lee SI. Nurses' perceptions regarding disclosure of patient safety incidents in Korea: a qualitative study. Asian Nursing Research. 2019;13(3):200-8. PMID: 31173923


5. Ock MS, Choi EY, Jo MW, Lee SI. Evaluating the expected effects of disclosure of patient safety incidents using hypothetical cases in Korea. PLoS One. 2018;13(6):e0199017. PMID: 29902233



6. Ock MS, Lee SI. Disclosure of patient safety incidents: implications from ethical and quality of care perspectives. Journal of the Korean Medical Association. 2017;60(5):417-27. 

7. Esswood J, Olley R. The implementation of open disclosure in Asian culture in Singapore: a systematic literature review. Asia Pacific Journal of Health Management. 2006;14(3):i299. 
8. Ock MS, Lim SY, Jo MW, Lee SI. Frequency, expected effects, obstacles, and facilitators of disclosure of patient safety incidents: a systematic review. Journal of Preventive Medicine and Public Health. 2017;50(2):68-82. PMID: 28372351




9. McLennan S, Beitat K, Lauterberg J, Vollmann J. Regulating open disclosure: a German perspective. International Journal for Quality in Health Care. 2012;24(1):23-7. PMID: 22140192


10. Ock M, Lee SI. Disclosure of patient safety incidents: implications from ethical and quality of care perspectives. Journal of the Korean Medical Association. 2017;60(5):417-27. 

11. O'Connor E, Coates HM, Yardley IE, Wu AW. Disclosure of patient safety incidents: a comprehensive review. International Journal for Quality in Health Care. 2010;22(5):371-9. PMID: 20709703


12. Ock M, Kim HJ, Jo MW, Lee SI. Perceptions of the general public and physicians regarding open disclosure in Korea: a qualitative study. BMC Medical Ethics. 2016;17(1):50-62. PMID: 27542889




13. Ministry of Health and Welfare, Korean Institute for Healthcare Accreditation. The korean institute for healthcare accreditation guideline (the third round). Sejon, Seoul. Korea: Ministry of Health and Welfare, Korean Institute for Healthcare Accreditation; 2018.
14. Ministry of Health and Welfare. Patient safety Plan (2018-2022). Sejong, Korea: Ministry of Health and Welfare; 2018.
15. Pyo JH, Choi EY, Lee W, Jang SG, Park YK, Ock MS, et al. Korean physicians’ perceptions regarding disclosure of patient safety incidents: a cross-sectional study. PLoS One. 2020;15(10):e0240380. PMID: 33031473



16. Ghalandarpoorattar SM, Kaviani A, Asghari F. Medical error disclosure: the gap between attitude and practice. Postgraduate Medical Journal. 2012;88(1037):130-3. PMID: 22282741


17. Keane D, Lang AR, Craven M, Sharples S. The use of vignettes for conducting healthcare research. Advances in Human Aspects of Healthcare. 2012.
18. Adams MA, Elmunzer BJ, Scheiman JM. Effect of a health system's medical error disclosure program on gastroenterology-related claims rates and costs. Official Journal of the American College of Gastroenterology. 2014;109(4):460-4. PMID: 24698856



19. Kachalia A, Kaufman SR, Boothman R, Anderson S, Welch K, Saint S, et al. Liability claims and costs before and after implementation of a medical error disclosure program. Annals of Internal Medicine. 2010;153(4):213-21. PMID: 20713789


20. Ock MS, Jo MW, Choi EY, Lee SI. Patient safety incidents reported by the general public in Korea: a cross-sectional study. Journal of Patient Safety. 2020;16(2):e90-6. PMID: 29894439


21. Weaver SJ, Lubomksi LH, Wilson RF, Pfoh ER, Martinez KA, Dy SM. Promoting a culture of safety as a patient safety strategy: a systematic review. Annals of Internal Medicine. 2013;158(5_Part_2):369-74. PMID: 23460092


22. Kim CW, Myung SJ, Eo EK, Chang Y. Improving disclosure of medical error through educational program as a first step toward patient safety. BMC Medical Education. 2017;17(1):52-7. PMID: 28259161










